Ahmedabad
(Head Office)Address : 506, 3rd EYE THREE (III), Opp. Induben Khakhrawala, Girish Cold Drink Cross Road, CG Road, Navrangpura, Ahmedabad, 380009.
Mobile : 8469231587 / 9586028957
Telephone : 079-40098991
E-mail: dics.upsc@gmail.com
Anti-microbial resistance
News: Recently, a survey conducted by the National Centre for Disease Control (NCDC) highlighted several key findings regarding the prescription and use of antibiotics in hospitals amidst growing concerns about Antimicrobial Resistance (AMR).
Key Findings:
• Preventative Use of Antibiotics: Over half of the surveyed patients (55%) were prescribed antibiotics for prophylactic indications, meant to prevent infections, rather than for therapeutic purposes (45%) to treat infections.
• Antibiotic Prescription Patterns: Only a small fraction (6%) of patients were prescribed antibiotics after a confirmed diagnosis of the specific bacteria causing their illness (definitive therapy), while the majority (94%) were on empirical therapy, based on the doctor’s clinical assessment of the likely cause of the illness.
• Lack of Specific Diagnosis: 94% of patients received antibiotics before a definitive medical diagnosis was confirmed, highlighting the prevalent use of antibiotics without precise knowledge of the infection\'s cause.
• Variation Among Hospitals: There were wide variations in antibiotic prescription rates among the hospitals, ranging from 37% to 100% of patients being prescribed antibiotics. A significant proportion (86.5%) of the prescribed antibiotics were administered through the parenteral route (not orally).
• Drivers of AMR: The NCDC survey notes, that one of the main drivers for the development of antibiotic resistance is the excessive and inappropriate use of antibiotics.
What is AMR?
• Antimicrobial resistance is the resistance acquired by any microorganism (bacteria, viruses, fungi, parasites, etc.) against antimicrobial drugs (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics) that are used to treat infections.
• As a result, standard treatments become ineffective, infections persist, and may spread to others.
• It is a natural phenomenon as bacteria evolve, making drugs used to treat infections less effective.
• Microorganisms that develop antimicrobial resistance are sometimes referred to as “superbugs”.
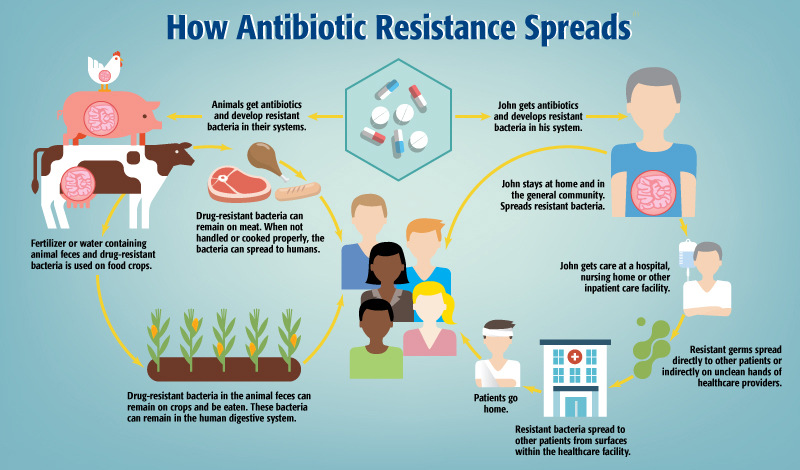
What contributes to spread of AMR?
• High Prevalence of Communicable Diseases: High burden of communicable diseases, such as tuberculosis, diarrhoea, respiratory infections, etc. that require antimicrobial treatment.
• Overburdened Public Health System: This limits the laboratory capacity for etiology-based diagnosis and appropriately targeted treatment.
• Poor infection Control Practices: Hygiene lapses in hospitals and clinics facilitate the spread of resistant bacteria.
• Injudicious use: Overprescribing by doctors under pressure from patients (often self-medication), incomplete antibiotic courses, and broad-spectrum antibiotics used unnecessarily create selective pressure for resistant bacteria.
• Easy Access: Unregulated over-the-counter availability and affordability of antibiotics fuel self-medication and inappropriate use.
• Lack of Awareness: Low public understanding of AMR and proper antibiotic use encourages misuse.
• Limited Surveillance: Lack of adequate monitoring systems makes it difficult to track and understand the scope of AMR.
Impact on Healthcare
• AMR can render previously effective antibiotics ineffective against bacterial infections. This complicates the treatment of common illnesses like pneumonia, urinary tract infections, and skin infections, leading to prolonged illnesses, more severe symptoms, and increased mortality rates.
• Treating resistant infections often requires more expensive and prolonged therapies, increased hospital stays, and sometimes more invasive procedures. This leads to higher healthcare costs for individuals, healthcare systems, and governments.
• AMR makes certain medical procedures riskier. Surgeries, cancer chemotherapy, and organ transplants become more hazardous due to the increased risk of infections that are resistant to standard antibiotics.
• As resistance grows, the available arsenal of effective antibiotics diminishes. This limitation in treatment options may lead to a scenario where previously manageable infections become untreatable, reverting medicine to a pre-antibiotic era where common infections could be fatal.
Address : 506, 3rd EYE THREE (III), Opp. Induben Khakhrawala, Girish Cold Drink Cross Road, CG Road, Navrangpura, Ahmedabad, 380009.
Mobile : 8469231587 / 9586028957
Telephone : 079-40098991
E-mail: dics.upsc@gmail.com
Address: A-306, The Landmark, Urjanagar-1, Opp. Spicy Street, Kudasan – Por Road, Kudasan, Gandhinagar – 382421
Mobile : 9723832444 / 9723932444
E-mail: dics.gnagar@gmail.com
Address: 2nd Floor, 9 Shivali Society, L&T Circle, opp. Ratri Bazar, Karelibaugh, Vadodara, 390018
Mobile : 9725692037 / 9725692054
E-mail: dics.vadodara@gmail.com
Address: 403, Raj Victoria, Opp. Pal Walkway, Near Galaxy Circle, Pal, Surat-394510
Mobile : 8401031583 / 8401031587
E-mail: dics.surat@gmail.com
Address: 303,305 K 158 Complex Above Magson, Sindhubhavan Road Ahmedabad-380059
Mobile : 9974751177 / 8469231587
E-mail: dicssbr@gmail.com
Address: 57/17, 2nd Floor, Old Rajinder Nagar Market, Bada Bazaar Marg, Delhi-60
Mobile : 9104830862 / 9104830865
E-mail: dics.newdelhi@gmail.com